Harmony Health Group Accepts UHC Insurance for Addiction Treatment
The Harmony Health Group provides comprehensive and holistic care for individuals who find themselves experiencing a range of mental health and substance use concerns. We recognize the impact that behavioral health concerns can have on your day-to-day life, as well as your overall health and wellness. With locations scattered along the East Coast, we have treatment facilities in Florida, Massachusetts, New Jersey, North Carolina, and Tennessee.
We are happy to provide in-network services for individuals with various health insurance policies, including United Healthcare. Our treatment facilities accept insurance coverage for our mental health, substance use, and dual diagnosis programs to help reduce the out-of-pocket costs associated with mental health treatment. If you would like to learn more about our United Healthcare addiction treatment services, we encourage you to call (866) 461-4474.
Check Your UHC Addiction Treatment Coverage Levels with Harmony Health Group
You can check your insurance coverage levels by calling us on: (866) 461-4474
Who is the Insurance Provider United Healthcare (UHC)?
United Healthcare (UHC) was founded in 1977 and has since grown to be one of the largest and most commonly used health insurers in the United States. When it was founded, UHC focused on providing healthcare plans for employers. Today, UHC offers a wide range of health services for individuals, families, and businesses.
Throughout its progression, UHC has introduced numerous innovative services for its members, including telemedicine options, wellness programs, and advanced care coordination for chronic diseases. UHC is committed to providing effective and innovative care for its policyholders. Because of their dedication, they have been named one of the World’s Most Admired Companies by Fortune and received the National Committee for Quality Assurance (NCQA) commendations for their Medicare and Medicaid plans.
A Few UnitedHealthcare Additional Brands and Services
What is a Behavioral Health Condition?
Behavioral health conditions can affect your overall physical and emotional well-being. Several conditions fall into this category, including mental health disorders, substance use disorders, and continuous engagement in behaviors that can cause problems in your life. These conditions affect everyone differently, which often requires different forms of treatment.
The key difference between behavioral health and mental health concerns is that mental health concerns are laid out and described in the DSM-V, which is a commonly used resource by mental health professionals. Behavioral health conditions can be treated with the use of various evidence-based practices, including cognitive-behavioral therapy (CBT), dialectical-behavioral therapy (DBT), and motivational interviewing (MI). Treatment can occur in both inpatient and outpatient treatment settings, allowing you to receive the care you need during different stages of your healing journey. If you have been struggling with a behavioral health condition, we encourage you to call (866) 461-4474 today to learn more about our available United Healthcare addiction treatment services near you!
What is a Drug Addiction or Substance Use Disorder (SUD)?
Substance use disorders (SUD) are mental health disorders that are known for making it challenging or nearly impossible to control, reduce, or limit the use of drugs and alcohol. SUDs are individualized, complex, and progressive mental health conditions that often require intense and personalized care for long-lasting sobriety.
Though there may be individual differences based on the individual and the substance being abused, some of the common signs or symptoms of an addiction include:
- Developing a tolerance
- Experiencing withdrawal symptoms
- Using in dangerous situations or putting yourself at risk
- Continuing use despite the challenges it has created in your life
- Struggling to maintain a level of functioning at work or school
- Inability to fulfill major roles and obligations
Another personal difference that can occur is the presence of other mental health conditions. The Substance Abuse and Mental Health Services Administration (SAMHSA) reported that over 21.5 million individuals in the U.S. were living with co-occurring disorders such as anxiety, depression, bipolar disorder, and ADHD. For many, these conditions are intertwined, which can work to your benefit and make recovery more challenging. Some individuals can tell you which condition was present first, while others struggle with a simple “chicken or the egg” real-life example. Regardless of how their mental health conditions develop, dual diagnosis care is the gold standard of care for those who are struggling with co-occurring mental health conditions.
What is Alcohol Addiction or Alcohol Use Disorder (AUD)?
An alcohol use disorder is a specific substance use disorder marked by excessive and typically uncontrollable alcohol use. Individuals living with an AUD often struggle to reduce, stop, or limit their use of alcohol. They may even have attempted to stop drinking before and found it difficult to maintain sobriety.
Alcoholism is an addiction that can be observed around the world and traced back to the time of the Greeks. If you’re struggling with AUD, it’s important to consult a medical professional before you attempt to reduce or stop your drinking because withdrawal symptoms can come with serious health concerns and complications. Individuals who are struggling with AUD often benefit from detoxification programs, inpatient care, and outpatient programming, depending on their symptoms. The Food and Drug Administration (FDA) has approved medications to treat AUD, which can be used to help manage withdrawal symptoms and reduce the frequency of cravings. If you have found it challenging to control or cut down on your drinking, we invite you to contact us today to learn about how our treatment programs can help you turn over a new leaf!
National Statistics on Alcohol and Drug Abuse
Does UHC Cover Inpatient Treatment for Drug and Alcohol Addiction?
Yes! United Healthcare generally provides coverage for inpatient alcohol and drug abuse treatment. This coverage ensures that their policyholders have access to the care that they need when they need it. Coverage for inpatient programs is dependent on symptoms and the level of impairment that you are experiencing.
Insurance providers, including UHC, are required to provide coverage for policyholders under the 2010 Affordable Care Act. This legislation ensures that health insurance companies provide coverage for essential health services, more specifically, inpatient psychiatric care, psychotherapy, and addiction treatment programs. Inpatient programs are often used by those struggling with addiction because they provide you with comprehensive care in a supportive and substance-free environment. Individuals who have been struggling to stop using or maintain sobriety are encouraged to contact us to see if our inpatient treatment programs could provide you with the care you need to effectively build a foundation for your recovery.
Does United Healthcare Provide Coverage for Outpatient Treatment for Drug and Alcohol Addiction?
Yes! UHC generally provides coverage for outpatient drug and alcohol treatment. Outpatient programs can help you stay connected to professionals and maintain a recovery-orientated schedule during the early stages of your recovery. Outpatient programs come in various intensities, providing comprehensive care during different stages of your recovery.
It is important to note that while UHC and other insurance companies provide coverage for outpatient programming, you need to verify your coverage to learn the exact details of your policy. UHC offers various healthcare options, allowing its members to choose coverage that aligns with their health needs within their budget. Differences within plans can be observed in the amount of coverage you receive and your out-of-pocket expenses. These expenses could come in the form of deductibles, premiums, and copayments. Additionally, some plans require the use of prior authorizations and have limitations or exceptions laid out in their plan.
Does UnitedHealthcare Cover Dual Diagnosis Treatment?
In most cases, yes, UHC provides coverage for some, if not more, of the costs associated with dual diagnosis treatment. Dual diagnosis treatment is the most effective approach for those who are living with more than one mental health condition because it provides simultaneous care, addressing both concerns at the same time.
For those who are struggling with substance use disorders and other mental health conditions, dual diagnosis care often includes additional programming added to their existing treatment schedule. Depending on your needs, this may include additional group therapy, support groups, individual sessions, and the use of psychotropic medications. Your clinical team will work with you to find a treatment approach that provides you with customized care that helps you develop the skills you need to effectively cope with and manage all of your mental health concerns.
Does United Healthcare (UHC) Cover Drug & Alcohol Treatment and Rehab?
United Healthcare is known for providing comprehensive coverage for its members, which generally means providing coverage for treatment options that can be used during various stages of addiction and recovery. For the most effective care, treatment plans should be tailored to each individual, including the intensity, duration, and frequency of care. Commonly used addiction treatment programs by UHC members include:
UHC Coverage for Alcohol Addiction Treatment
UHC Coverage for Drug Addiction Treatment
UHC Coverage for Addiction Treatment Testing
Harmony offers a multitude of locations up and down the East Coast for behavioral health services. Call us to learn about our facilities and treatment options.
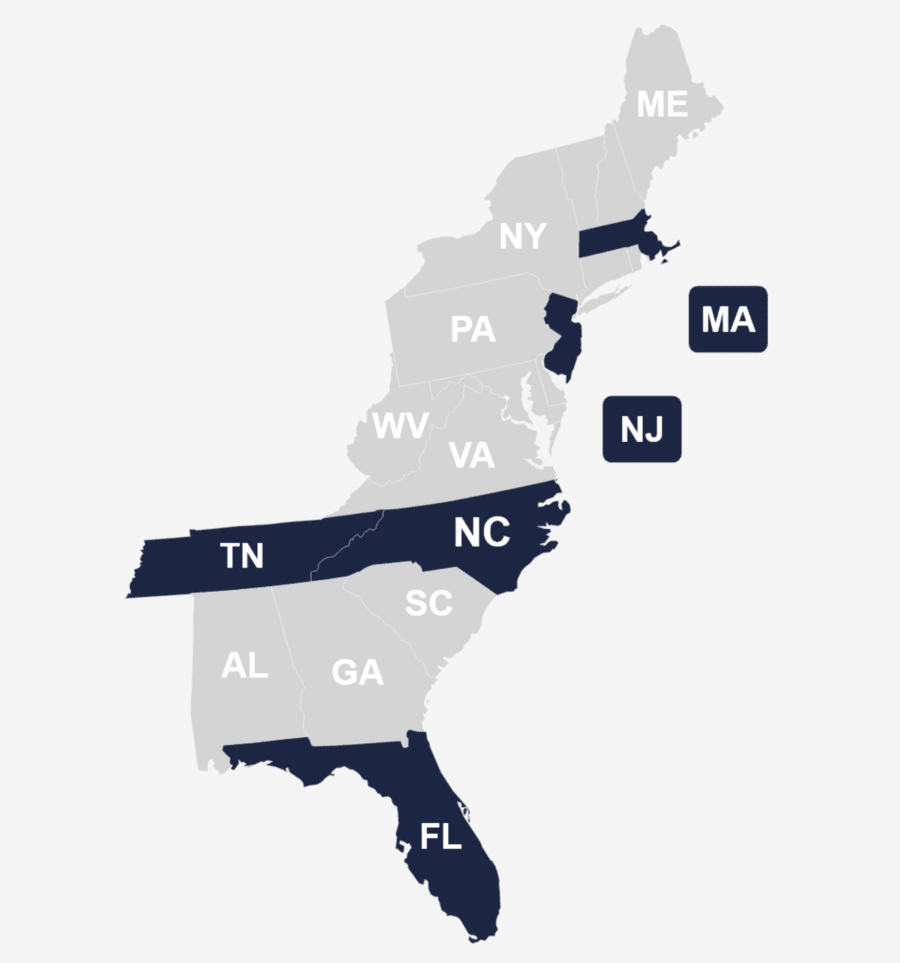
Addiction Treatment Programs That Take UnitedHealthcare Near Me
Individuals who need addiction treatment may wonder if United Healthcare covers addiction treatment therapy. The first step to ensuring that you can take advantage of your coverage is to find a UHC provider. You can do this with a simple online search using keywords like “UHC addiction treatment providers near me.”
The Harmony Health Group is a leading behavioral health treatment provider along the East Coast with various treatment programs for those who are experiencing substance use and mental health. Our Addiction Counselors are waiting to learn about your experiences and concerns so that they can match you with your ideal treatment program. Contact us today to get started!
UHC Covered Drug & Alcohol Addiction Treatment Options in FL
UHC Covered Drug & Alcohol Addiction Treatment in MA
UHC Covered Drug & Alcohol Addiction Treatment in NC
UHC Covered Drug & Alcohol Addiction Treatment in NJ
UHC Covered Drug & Alcohol Addiction Treatment Options in TN
UHC Drug & Alcohol Addiction Provider and Referral Network
UnitedHealthcare has a comprehensive drug and alcohol addiction provider and referral network, which provides access to a wide range of treatment options for policyholders. Available options typically include providers within detoxification programs, inpatient rehabs, outpatient programs, and medication-assisted treatment providers to support you in your sobriety.
UHC’s extensive network connects members with accredited facilities and professionals specializing in addiction treatment. This network is designed to ensure that members receive high-quality care tailored to their specific needs. Additionally, UHC provides resources and referrals to help members find the most appropriate treatment programs and providers in their area. The Harmony Health Group is pleased to have multiple treatment facilities with the UHC provider network.
Contact Us
Check Your UHC Insurance Coverage for Substance Use Disorder and Alcohol Use Disorder Treatment
To check your UHC insurance coverage for addiction treatment, we encourage you to review your policy documents or contact UHC directly. This allows you to understand the scope of your coverage and how it applies to addiction treatment programs. Understanding your coverage is essential for you to plan and understand your potential out-of-pocket expenses.
You can also use UHC’s online portal to verify your benefits and coverage details. If you have questions or need assistance, we encourage you to reach out to our Admission Counselors for support. We are familiar with UHC’s policies and can help you navigate the process. Call us today to explore your United Healthcare addiction treatment coverage options.
How To Get United Healthcare To Pay For Behavioral Health and Substance Abuse Treatment Near Me
Once you have reached a point in your journey where you are ready to get help, it makes sense that you would then wonder about how to get United Healthcare to pay for your treatment. The first step is to see if you’re required to choose an in-network provider or not. This can be determined when you verify your coverage.
During the admission process and throughout your treatment, the treatment facility will submit medical claims to UHC directly for you. They will also track authorizations if they are required to reduce challenges that you may experience. With your provider managing your medical claims, you can focus on fully participating in your treatment. Our team will keep you updated about your claims process and let you know if there are any concerns along the way.
Statistics on UHC Drug and Alcohol Addiction Treatment in the United States
Sources
Get in touch with Harmony Health Group to find out about our rehab admissions process, free assessment, treatment options or to check your insurance coverage levels. Your first step to recovery starts here!
Provide Your Contact Details
8520 Cliff Cameron Dr. Ste 450, Charlotte, NC 28269
