Harmony Health Group Accepts Optum Insurance
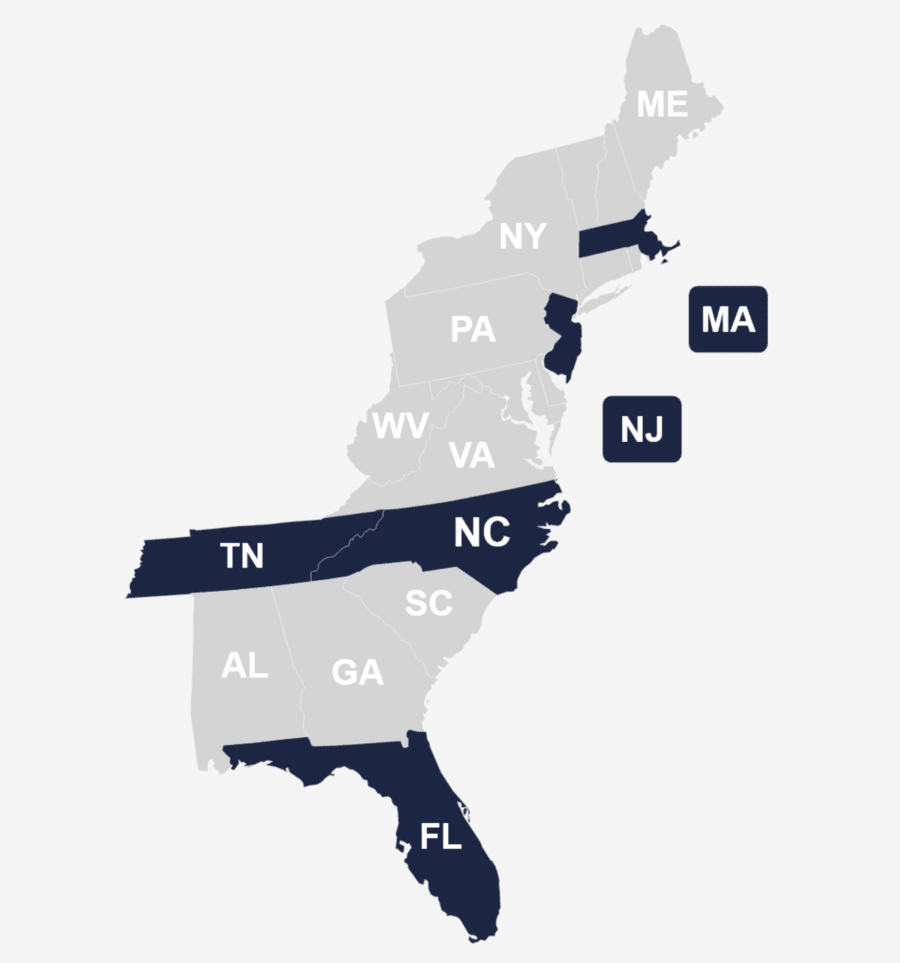
Harmony Health Group operates multiple rehabilitation facilities spanning several states, including Florida, Massachusetts, North Carolina, New Jersey, and Tennessee. We deliver extensive care to those struggling with substance abuse, mental health, and dual diagnosis challenges through diverse services tailored to meet the unique needs of our clients.
In our commitment to enhancing accessibility and affordability of care, we’re in-network with various insurance providers, including Optum. Harmony Health Group strives to eliminate financial obstacles by embracing insurance coverage, ensuring access to high-quality treatment without unnecessary financial burdens. If you or someone you know is in search of addiction rehabilitation or mental health support and has Optum Insurance, Harmony Health Group is a reliable choice for comprehensive and covered care.
Check Your Optum Coverage Levels with Harmony Health Group
You can check your insurance coverage levels by calling us on: (866) 461-4474
We’re here to listen. Let’s talk today.
What is Optum Rehab Coverage?
Optum rehab coverage for substance abuse and addiction provides financial support for services related to treatment. If you or a loved one is grappling with alcoholism or drug abuse, Optum can assist in covering the costs associated with rehabilitation services, including detoxification, counseling, and therapy.
Optum offers a comprehensive approach to rehab coverage that may include coverage for inpatient and outpatient care and support to access a range of evidence-based treatments tailored to your unique needs. Review your specific Optum plan to understand the extent of coverage for Optum alcohol rehab and Optum drug rehab and any potential out-of-pocket expenses, like copayments, deductibles, and exclusions. Seeking help for substance abuse is a significant step, and with Optum’s rehab coverage, you can embark on a path toward recovery.

Some Various Optum Insurance Brands, Products, & Services
Does Optum Cover Rehab?
Yes, Optum employs a compassionate team of care advocates and peer support specialists, utilizing innovative analytics and programs aimed at fostering relationships with the insured, the providers, and their communities as part of its holistic approach. Rehabilitation coverage details will vary from plan to plan.
Contact Harmony Health Group at (866) 461-4474 for more information and coverage specifics related to your distinct needs for rehabilitation.
Does Optum Cover Mental Health Treatment Near Me?
Optum typically covers mental health treatment, offering a comprehensive range of services. Whether you are looking for counseling, therapy, or other mental health interventions, Optum’s network includes providers and facilities that can address your needs. Review your particular plan for details on coverage, providers, and any potential out-of-pocket expenses related to mental health treatment in your local area.
Call (866) 461-4474. Our dedicated team at Harmony Health Group can provide an understanding of your benefits as they apply to your specific needs so you can maximize the financial support on your path toward recovery.
Mental Health-Related Services Covered by Optum Insurance
Drug & Alcohol Addiction Inpatient and Outpatient Rehab Centers That Take Optum Insurance
Harmony Health Group runs numerous drug and alcohol addiction treatment facilities in different states, delivering extensive inpatient and outpatient rehabilitation services. These centers that accept health insurance are dedicated to guiding individuals on the journey to recovery, featuring specialized programs tailored to address substance abuse, mental health, and dual diagnosis issues. Click on the links below for more information:
- Harmony Treatment and Wellness
- Recovery By The Sea
- Recovery In Tune
- Blue Hills Recovery
- Serenity At Summit: New England
- Harmony Recovery Center
- Midwood Addiction Treatment
- Harmony Healing Center
- Summit Behavioral Health: Princeton Junction
- Serenity at Summit: Union
- Harmony Oaks Recovery Center
- Summit at Harmony Oaks Recovery Center
- Summit Detox
Does Optum Insurance Cover Residential Treatment?
Optum typically covers residential treatment for those seeking intensive care and support for various mental health and substance abuse issues. Residential treatment, or inpatient care, involves residing at a treatment facility to receive 24/7 care and therapy. Reviewing your specific Optum plan to understand the extent of coverage, any potential requirements and associated costs related to residential treatment is important.
Call (866) 461-4474 for assistance in navigating your insurance coverage details.
Does Optum Cover Medical Detox Treatment?
Optum insurance commonly includes coverage for medical detoxification treatment, offering financial assistance for supervised withdrawal from substances. This vital phase in addiction recovery involves medical oversight to ensure a safe withdrawal process. Optum’s commitment to holistic care encompasses coverage for medical detox, demonstrating its dedication to supporting individuals through every essential stage of substance abuse treatment.
It’s recommended to thoroughly review the specifics of your Optum plan to grasp the extent of coverage, potential prerequisites, and any associated costs linked to medical detox.
Does Optum Cover Mental Health Therapy Treatment?
Optum provides coverage for certain mental health therapy treatment costs. The extent of coverage depends on your specific plan, encompassing factors such as in-network providers, session limits, and potential copayments or deductibles. For detailed information about your plan, including mental health therapy coverage, contact us.
Emphasizing a commitment to mental and emotional well-being, Optum offers a variety of therapy options to bolster psychological health. Whether through behavioral health solutions for Medicaid or tailored offerings for employers, Optum ensures some level of coverage for mental health, underlining its dedication to supporting mental health.
Mental Health Therapy Programs Covered by Optum
Does Optum Insurance Cover Eye Movement Desensitization and Reprocessing (EMDR) Therapy?
Optum Health Insurance typically covers Eye Movement Desensitization and Reprocessing (EMDR) therapy. This structured eight-phase process includes elements like history-taking, treatment planning, and bilateral stimulation to facilitate the adaptive processing of traumatic memories. EMDR aims to promote healing and reduce the impact of trauma on mental health.
While coverage specifics vary, Optum consistently supports EMDR therapy as part of its comprehensive mental health care commitment. To understand coverage details, potential requirements, and associated costs, carefully review your insurance plan or call (866) 461-4474.
Learn About Harmony Health Group’s Drug & Alcohol Rehab Center Locations
Harmony Health Group is committed to guiding individuals on the path to overcoming addiction and maintaining lasting sobriety. Offering empathetic care and personalized solutions, explore the rehabilitation centers that accept Optum, outlined below. For more details and personalized support on your journey towards a healthier, more fulfilling life, call (866) 461-4474.
Treatment Centers in Florida (FL) That Take Optum Insurance
Treatment Centers in Massachusetts (MA) That Take Optum Insurance
Treatment Centers in North Carolina (NC) That Take Optum Insurance
Treatment Centers in New Jersey (NJ) That Take Optum Insurance
Treatment Centers in Tennessee That Take Optum Insurance
Harmony offers a multitude of locations up and down the East Coast for behavioral health services. Call us to learn about our facilities and treatment options.
How To Check Optum Insurance Coverage Levels for Addiction Treatment Near Me
For assistance verifying your rehab treatment coverage with Optum, we invite and encourage you to contact our team directly. We are dedicated to offering personalized support and assisting you in comprehending the details of your coverage so that you can make informed decisions. Connect with our friendly and professional staff by calling (866) 461-4474 today.
Alternatively, your insurance coverage levels can be assessed through our online form below. By following the steps, you’ll acquire the essential information to embark on your path to wellness confidently. We aim to ensure you a seamless, stress-free, and transformative experience.
Other Addiction Treatment Programs Covered by Optum Insurance
Explore a variety of addiction treatment programs often covered by Optum and provided by Harmony Health Group. The upcoming sections will briefly delve into distinct programs, offering glimpses into the therapeutic methods accessible to aid your journey toward enduring recovery and well-being. Dial (866) 461-4474 for a deeper exploration into our addiction treatment programs and how your Optum plan applies.
Optum Insurance Coverage for Partial Hospitalization Programs (PHP)
Optum Insurance Coverage for Inpatient Rehab
Optum Insurance Coverage for Intensive Outpatient Program (IOP)
Optum Insurance Coverage for Acute Treatment Programs
How Much is Rehab with Optum Insurance Near Me?
Navigating the financial aspects of Optum rehab coverage is a personalized journey influenced by factors such as your plan details and the chosen rehabilitation program. On average, individual drug rehabilitation costs approximately $13,475. For detailed insights into out-of-pocket expenses, deductibles, copayments, and other policy details, contact Harmony Health Group at (866) 461-4474.
We are committed to supporting your journey to recovery. Connect with us for a customized understanding of rehabilitation costs tailored to meet your distinct treatment needs. Our team offers professional, transparent, and friendly assistance, guiding you through the financial considerations of your recovery.
How To Get Optum Insurance to Pay for Drug & Alcohol Rehab Treatment
To initiate the process of getting Optum to cover drug and alcohol rehab treatment, thoroughly review your policy. Familiarize yourself with the specific coverage details, including limitations, in-network providers, potential out-of-pocket expenses, and affordable programs. It’s crucial to understand the scope of your benefits and whether the chosen rehab facility and treatment services align with your Optum benefits.
Next, contact Optum directly or call (866) 461-4474 to verify your coverage and seek guidance on the prior authorization process. Obtaining prior authorization ensures that the insurance provider reviews and approves the proposed rehab treatment plan, increasing the likelihood of coverage. Keep in mind that providing clear documentation of medical necessity, such as assessments and recommendations from healthcare professionals, can strengthen your case for coverage approval.
By actively engaging with Optum, understanding your policy, and following the necessary procedures, you enhance your chances of getting your insurance provider to pay for drug and alcohol rehab treatment.
National Statistics on Drug & Alcohol Rehab and Optum Health Insurance Claims
- Optum’s expansive behavioral health network encompasses over 39,000 telemental health providers in all 50 states.
- Over 90% of Optum-insured members reside within a 20-mile radius of a medication-assisted treatment (MAT) provider.
- Utilizing proprietary algorithms, Optum evaluates combinations of comorbidities to steer individuals toward a suitable level of care. This process involves assessing 18,000 or more criteria.
- By integrating the Optum Employee Assistance Program with Behavioral Health, employees are seamlessly connected to the necessary care, resulting in a 22% reduction in outpatient care costs and 18% fewer outpatient visits.
- More than half of the transactions processed through Optum’s Provider Express are entirely automated, leading to expedited attestations, credentialing applications, and claims, allowing healthcare providers to prioritize patient care.
- By collaborating with providers and the local community, the Optum/UnitedHealthcare Community Plan model has showcased enhanced outcomes in various behavioral health measures in Tennessee. This includes a 12% reduction in statewide inpatient utilization, resulting in savings of $3.6 million, and an 8.3% decrease in psychiatric readmissions, leading to savings of $1.0 million.
- In the initial months of the pandemic, the number of providers offering virtual behavioral health visits increased from 6,500 to more than 10,000. By the sixth month of the pandemic, over 20,000 providers had completed attestation to be included as virtual visit providers.
- Analyzing Optum claims data spanning from June 2021 to May 2022 revealed the predominant substance use disorders in the United States, with alcohol ranking as the most prevalent, closely followed by opioids.
- According to a recent study by Optum, the expenses for out-of-network residential treatment amount to an estimated $44,000 per 90-day episode for both employers and employees, in contrast to $13,000 for the same treatment provided by in-network providers.
Get in touch with Harmony Health Group to find out about our rehab admissions process, free assessment, treatment options or to check your insurance coverage levels. Your first step to recovery starts here!
Provide Your Contact Details
8520 Cliff Cameron Dr. Ste 450, Charlotte, NC 28269
